Associated conditions
Useful info on conditions linked to scleroderma
Find out more
Lichen sclerosus also occasionally affects other areas of the body, including the upper arms, back, breasts and shoulders. It is most common in women who have been through the menopause, although it can also occur in men as well as in children. LS is not an infection and cannot be spread to your partner or to anyone else. It is not clear what causes LS, however it is thought to be related to overactivity of the immune system. Family history may sometimes be a factor, with rare cases of several people being affected within the same family group.
Although it can be uncomfortable and distressing, LS is usually treatable. This means that it will usually be possible to control the symptoms with simple treatments.
In women and girls, LS tends to affect the vulva (the skin around the entrance to the vagina) and the skin around the anus (back passage). Friction or damage to the skin can trigger the problem and make it worse. This is called a 'Koebner response'. Irritation from urine leakage or from wearing incontinence pads or pantyliners can also aggravate the LS. Symptoms can include:
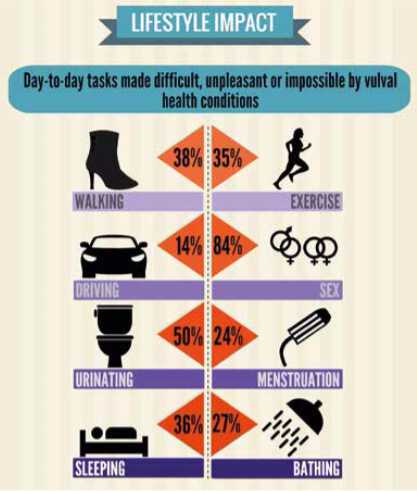
Without treatment, the vulva may gradually scar and shrink. This can make the entrance to the vagina narrower, with sex becoming increasingly difficult and painful. In most cases, although any patches on the general skin surface will not feel persistently itchy, those in the genital area usually do, and can also become sore if the skin breaks down or cracks. The scar-like process can tighten the skin, leading to problems with urination and sexual intercourse. Tightening of the skin around the anus can also lead to constipation issues.
In men and boys, LS tends to develop on the foreskin and the end of the penis, although the skin around the anus is rarely affected. Symptoms can include:
For both men and women, it is often easy for a doctor to diagnose LS by asking about your symptoms and examining your skin. However, in some cases, a very simple procedure known as a biopsy, where a skin sample is taken for analysis, may be needed to make a firm diagnosis.
For most people, LS is a long-term condition that lasts for many years and may flare up and down over time. There is presently no cure, but symptoms can normally be controlled with steroid medication applied directly to the affected skin. Occasionally, LS goes away on its own and does not come back, but this usually only occurs when children with the condition reach puberty.
The main treatment for LS is steroid ointment or cream, which helps to control symptoms. It should be applied regularly, but relatively sparingly, to the affected areas of skin. Your doctor will advise you on how much to use, how frequently, and for how long. Generally, a 30g tube should last for around three months. When used appropriately, the risk of side effects such as thinning of the skin is very low. Symptoms tend to ease after a few weeks of treatment, but it may be a few months before your symptoms are fully under control. Steroid creams and ointments are very effective in most cases, however, if these do not relieve symptoms, other treatments may be suggested by a specialist.
In a few cases, surgery may be needed to treat problems caused by LS. For example, a small operation may be carried out to divide adhesions if the skin sticks together. If the condition causes a woman's vaginal opening to become very narrow and affecting sex, surgery to widen it may be suggested. Men or boys may need a small operation to remove the foreskin if steroid ointments or creams do not help and the foreskin becomes severely affected. This can result in the condition settling fully.
For women who find sex painful, it may help to use a lubricant or a vaginal dilator. There is a very small increased chance of developing cancer of the vulva or penis if you have lichen sclerosus. If any skin change develops which does not respond to steroid creams, in particular any skin thickening, soreness or ulceration lasting for more than two weeks, you need to tell your doctor without delay. You may need a biopsy to test for skin cancer.
With thanks to the British Association of Dermatologists (BAD), the Association of Lichen Sclerosus and Vulval Health and NHS Choices for assisting with the content and imagery supplied for the article.
In addition to medical treatments, there are a number of other measures that can help keep your symptoms under control:
We would like to thank Colette for sharing her personal experience of her diagnosis and of living with this intimate and little-known condition.
By talking about rare conditions like LS, we aim to increase awareness and improve diagnosis rates, enabling more people to benefit from appropriate treatments and improved quality of life.
Collette shares her personal experiences of her family history and of subsequently receiving a diagnosis of LS herself; as well as having to deal with the treatment and management of this often challenging condition on an ongoing basis.
Read Colette's full story here.

Useful info on conditions linked to scleroderma
Find out more
Have a look at the SRUK shop for products to keep you warm including gloves and socks.
Find out more
Sign-up to receive your monthly Raynaud's and Scleroderma E-News direct to your inbox.
Find out more