Tuesday 23rd April 2024
RAIRDA Survey
Have your say on the way your services are working for your Rare Autoimmune Rheumatic Disease (RAIRD)
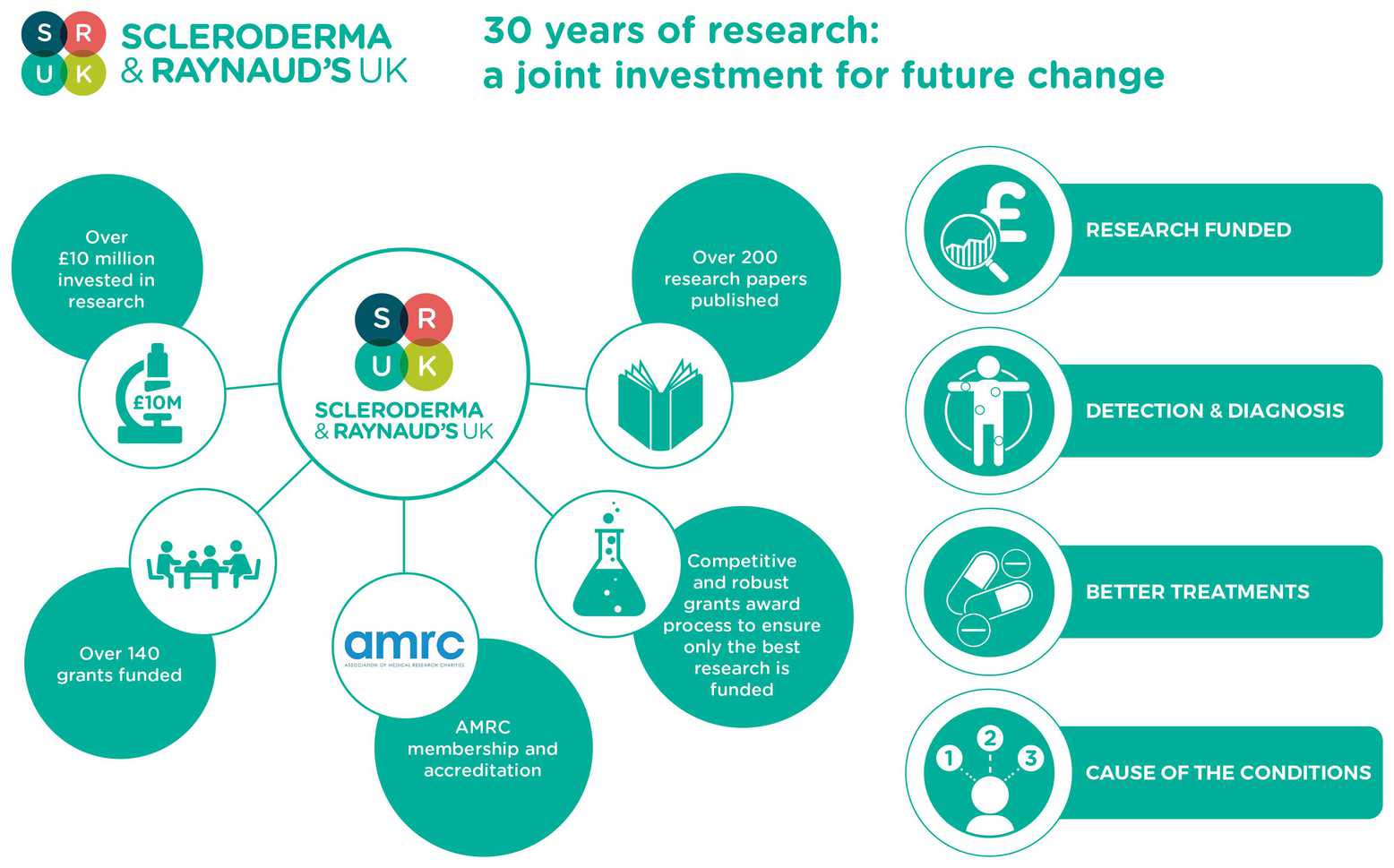
SRUK has a 30 year legacy of supporting vital research into Scleroderma and Raynaud’s phenomena. We have made it our mission to transform outcomes for patients, injecting much needed funding into highly promising research areas.
SRUK has a 30 year legacy of supporting vital research into Scleroderma and Raynaud's phenomena. Existing originally as the two founding charities, the Raynaud's and Scleroderma Association (RSA) and the Scleroderma Society, and eventually coming together to achieve more. We have made it our mission to transform outcomes for patients, injecting much needed funding into highly promising research areas.
We've come a long way since 1985, when a diagnosis of scleroderma meant that you had a 60% chance of surviving more than 5 years. Now, in 2018, a diagnosis of scleroderma does not have to be so scary. The survival rate has gone up to 85%, and even more amazingly survival post renal failure has dramatically increased from 25% to 80%.
We also now have 6 specialist centres in England, some of which are providing support to other clinics to ensure that more people are receiving the appropriate treatment and care.
As part of our commitment to ensuring that our community is at the forefront of understanding the research that is carried out by our clinician researchers, we are publishing the'Inaugural Research Impact' Report. This report highlights how research has enabled the amazing progress that has been achieved over the last 30 years.
We've focused on four key areas:
As a special sneak peek for our community members, here are some highlights from the report.
Understanding the cause of Scleroderma and Raynaud's
A genome wide association study to get to the root of the problem
Professor Chris Denton, Royal Free Hospital/University College London
A team of world class scleroderma scientists at the Royal Free hospital made a breakthrough, uncovering a potential mechanism behind pulmonary hypertension, one of the biggest risk factors in scleroderma. They have spotted how certain genes may be behind blood vessel changes, potentially spotting those patients most at risk of this deadly complication.
Every single thing that a cell can do, from colouring your eyes through to conducting thoughts across your brain, depends on a detailed and complex instruction manual called the genome. There are thousands of different instructions (or genes) that make us who we are. Yet cells don't follow all the genes all the time. A nerve cell and a skin cell behave very differently, and this is because they subscribe to different parts of this instruction manual.
The symptoms of a disease occur because cells start to follow instructions that they normally ignore. Sometimes this is because the cells themselves are faulty, other times it is because something, perhaps a bacteria or virus, is stressing the cell, changing its behaviour. In scleroderma, something causes the immune system to begin attacking the body, and these attacks cause damage to the cells, which defend themselves by changing the genes they use. In areas of extreme damage where repair is impossible, the cells form scar tissue.
If we can understand which genes are in play for Scleroderma or Raynaud's, we can begin to anticipate how each person's disease will behave, and begin to explore ways to intervene or even correct the problem.
This is not a simple challenge, yet it is one to which Professor Chris Denton has devoted almost 25 years of research, becoming a world authority in the process. His work is improving the ability of doctors to predict how scleroderma may behave, identifying which patients will respond best to certain treatments and even helping to develop new treatments.
Using cutting-edge techniques to study the genes involved in different forms of scleroderma, Chris' team uncovered a cluster of active genes that normally help control blood vessels and may be linked to many symptoms of scleroderma, including pulmonary hypertension, a major risk-factor in diffuse systemic scleroderma.
They discovered that the highly specialised cells that normally line our blood vessels start to follow incorrect genetic instructions, transforming them into a different type of cell without some of their specialised properties. The consequence is that the barriers to the blood vessels become very leaky, contributing to pulmonary hypertension, possibly by allowing a type of white blood cell that helps form scar tissue to interact with the vital tissue.
These major advances in understanding the mechanisms and genes behind some of the most serious scleroderma symptoms has opened up many opportunities for trialing new treatments, opportunities that Chris' team are set up to build upon.
Enabling better diagnosis for Scleroderma
Staging Interstitial Lung Disease: A world class system for clinical diagnosis
Dame Carol Black, Professor Athol Wells, Professor Chris Denton, Royal Free/Royal Brompton
A team of world-leading clinicians and scientists developed a life-saving algorithm that allows clinicians to rapidly diagnose lung fibrosis as well as an expert. Led by Dame Carol Black and Professor Chris Denton from the Royal Free Hospital and Professor Athol Wells from the Royal Brompton, this dream-team's solution is one of the most important advances in scleroderma diagnosis in recent years.
In recent times fibrosis of the lungs has become the number one cause of death in people with systemic scleroderma. For people with the most severe lung disease it is important to treat aggressively, squashing the immune response. But these treatments are harsh and can have severe side-effects. It is therefore vital for doctors to know which patients have the most advanced lung fibrosis so they can treat appropriately.
Unfortunately the standard way of assessing lung function just wasn't good enough. There is too much variability, and the complexity of achieving an accurate understanding is beyond all but the most experienced doctors.
Dame Carol Black and her colleagues' approach was to combine High Resolution Computed Tomography, a technique that takes accurate cross-sectional x-rays of the body and reconstructs an internal view of the lungs, with standard tests of the lung's performance. The revolutionary element was to create an algorithm that can draw on this information and classify a patient's degree of lung disease severity. They developed this test by working with over 200 people with scleroderma, and then evaluated their final model. Incredibly, in the trials, doctors with less than 2 years' experience were able to classify the severity of disease in a way comparable to highly experienced radiologists after only 10 minutes training. This technique has put the ability to assess a potentially fatal aspect of scleroderma into the hands of doctors everywhere and has gone on to become the international standard for assessment, quite literally revolutionizing a vital part of scleroderma medicine.
Earlier detection of Scleroderma and Raynaud's
Nailbed micro capillaroscopy: A tool for earlier diagnosis
Dr Graham Dinsdale, University of Manchester
Scientists at the University of Manchester developed an essential diagnostic tool that can pick up the earliest signs of scleroderma in patients with Raynaud's Phenomenon. Led by Dr Graham Dinsdale, they overcame significant technical difficulties to develop a long sought-after method of spotting microscopic changes to the nailbed capillaries. This work has increased the chances of diagnosing early, helping to minimise the effects of the disease for many people.
The smallest blood vessels we have in our bodies are called capillaries. In normal Raynaud's these capilaries are unaffected, but if the disease is progressing into scleroderma, it leaves its first marks on the tiny capillaries, scarring and distorting them. Spotting this damage gives doctors the best chance to get on top of the disease, minimizing the window where lasting systemic damage can occur.
Unfortunately, spotting this capillary damage reliably is hard. All people are built slightly differently, with no typical'sign' of scleroderma. The solution is to monitor changes to the capillaries in the hand over time, but the hundreds of meters of capillaries in just one hand makes it hard to compare the same area. It is all too easy for doctors to miss the warning signs, and finding a way to help is a huge technical challenge.
This has changed. For 12 years a team of scientists at the University of Manchester, led by Dr Graham Dinsdale and Professor Ariane Herrick, have been tackling this challenge. Their breakthrough insight was to develop computer software that can weave individual images of capillaries into a detailed and highly reproduceable image. At a glance doctors can now see the entire nailbed, and compare it with the entire nailbed from a previous date to look for the signs of the disease. Our research has unlocked a solution that is equipping doctors with the tools they need to monitor people with Raynaud's, something which could be the difference between lifelong disability and a relatively normal life.
Developing the best treatments available
A topical treatment for calcinosis
Professor Richard Winpenny, University of Manchester
Calcinosis is a debilitating problem, not just in scleroderma but in other diseases like arthritis too. This team led a revolutionary project to develop a treatment that can dissolve them.
Calcinosis is the formation of painful, hard lumps over the skin, particularly at pressure points such as joints. Unsurprisingly this can be debilitating. Professor Richard Winpenny and Professor Ariane Herrick were interested in learning what these lumps are actually made of, and crucially, whether treatments can be given to dissolve them safely, and SRUK made this a reality, continuing their long tradition of identifying promising projects at an early stage and giving them a chance to flourish.
Using advanced chemistry, the team assessed various reagents that might have the necessary properties to dissolve calcinoids, combining them with a'nanotechnology' delivery system that can transport this chemical across the skin and into the calcinoid. The goal is now to make a topical treatment that can be easily applied and will rid a person of a painful condition.
Tuesday 23rd April 2024
Have your say on the way your services are working for your Rare Autoimmune Rheumatic Disease (RAIRD)
Tuesday 19th March 2024
The Scleroderma and Raynaud’s UK sponsored 'Science in Medicine School Teams Prize 2024' contest is now open for entries. The contest aims to engage sixth form school students with science in medicine, and challenges students to prepare an ePoster with a novel vision on how to promote the health and well-being of individuals with Scleroderma and/or Raynaud’s. If you're interested in entering, or know someone in sixth form who might be, read on to find out more!
Wednesday 28th February 2024
As high bills continue to threaten the health of those living with the debilitating condition; SRUK is appealing to energy companies to provide financial assistance to them.